Intro
Cardiovascular diseases (CVDs) continue to be the main motive of mortality worldwide, accounting for about 17.9 million deaths every year, according to the World Health Organization. Thrombosis, or the formation of blood clots, performs an imperative position in lots of cardiovascular events, including myocardial infarction (heart attack), ischemic stroke, and peripheral arterial sickness. The expertise and management of thrombosis have advanced appreciably, with platelet inhibition rising as a cornerstone in cardiovascular care.
Among the antiplatelet marketers used in clinical exercise, clopidogrel—a thienopyridine class drug—has garnered vast interest because of its efficacy, protection profile, and massive use. Approved via the U.S. Food and Drug Administration (FDA) in 1997, clopidogrel has since emerged as a mainstay in both number one and secondary prevention of thrombotic occasions. This article explores clopidogrel’s mechanism of motion, medical packages, blessings, obstacles, and destiny prospects in cardiovascular medication.
The Role of Platelets in Cardiovascular Disease
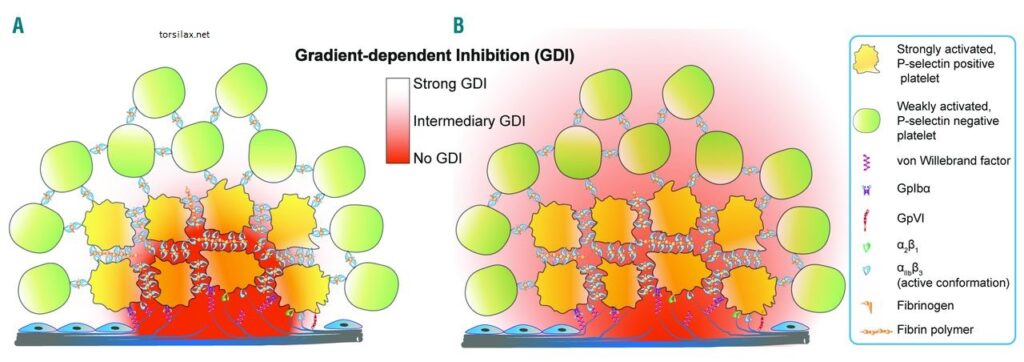
Platelets are small, anucleate cellular fragments derived from megakaryocytes inside the bone marrow. They play a vital function in hemostasis, forming plugs at sites of vascular damage. However, platelet aggregation can contribute to the pathogenesis of atherosclerotic plaque rupture and thrombus formation if it is dysregulated.
In situations like acute coronary syndromes (ACS), percutaneous coronary intervention (PCI), and cerebrovascular ischemia, irrelevant platelet activation can bring about catastrophic clinical outcomes. Therefore, inhibiting platelet aggregation reduces the chance of arterial thrombosis and its sequelae.
Clopidogrel: Pharmacology and Mechanism of Action
Clopidogrel is an oral antiplatelet remedy belonging to the thienopyridine magnificence. It is a prodrug, meaning it requires metabolic activation in the liver to become pharmacologically lively. Once metabolized mainly using Cytochrome P450 enzymes, especially CYP2C19, clopidogrel’s energetic metabolite irreversibly binds to the P2Y12 receptor on platelets. This binding inhibits adenosine diphosphate (ADP)-mediated activation of the glycoprotein GPIIb/IIIa complex, thereby preventing platelet aggregation.
The irreversible inhibition of the P2Y12 receptor persists for the lifespan of the platelet, generally 7 to 10 days. As such, its results are sustained even after the drug is discontinued; that’s attention in surgical planning.
Clinical Applications of Clopidogrel
Clopidogrel has a wide range of indications throughout cardiovascular care, both as monotherapy or in aggregate with other sellers, including aspirin in dual antiplatelet therapy (DAPT).
1. Acute Coronary Syndromes (ACS)
Clopidogrel is a general aspect within the control of non-ST-elevation myocardial infarction (NSTEMI) and ST-elevation myocardial infarction (STEMI). The landmark CURE trial (2001) demonstrated that including clopidogrel to aspirin substantially reduced cardiovascular loss of life, myocardial infarction, and stroke in ACS patients.
2. Percutaneous Coronary Intervention (PCI)
After PCI with stent implantation, the threat of in-stent thrombosis is high. Clopidogrel, in combination with aspirin, is usually recommended to reduce the chance of thrombotic complications. Guidelines commonly endorse DAPT for at least 6 to 12 months post-PCI, depending on the stent type and man or woman’s bleeding risk.
3. Ischemic Stroke and Transient Ischemic Attack (TIA)
Clopidogrel is powerful in lowering recurrent ischemic stroke. The CAPRIE trial (1996) compared clopidogrel to aspirin in patients with recent stroke, myocardial infarction, or peripheral arterial disease, displaying a modest, however statistically, sizeable advantage with clopidogrel.
4. Peripheral Arterial Disease (PAD)
Patients with PAD are at improved danger of cardiovascular activities. Clopidogrel improves outcomes by reducing thrombotic complications and improving arterial go-with-the-flow, making it a favored antiplatelet agent in many PAD cases.
Benefits of Clopidogrel
1. Proven Efficacy
Clopidogrel has verified consistent efficacy in reducing thrombotic activities in several large-scale medical trials, including CURE, CAPRIE, and COMMIT.
2. Well-Established Safety Profile
Clopidogrel is a safer option for sufferers at higher bleeding risk or the elderly compared to other P2Y12 inhibitors like prasugrel and ticagrelor.
3. Convenient Dosing and Availability
Clopidogrel is administered as soon as daily and is extensively available as a traditional remedy, making it accessible and cost-effective for long-term use.
Limitations and Challenges
1. Variable Response Due to Genetic Polymorphisms
A significant problem with clopidogrel is interindividual variability in its efficacy, mainly due to genetic polymorphisms in the CYP2C19 enzyme. Individuals with loss-of-characteristic alleles (e.g., CYP2C19 *2/2) have reduced potential to transform clopidogrel into its lively shape, resulting in resistance. This genetic variability can result in an elevated chance of negative cardiovascular consequences.
2. Delayed Onset of Action
Clopidogrel requires hepatic activation, which delays its onset of movement. In acute settings, a loading dose (typically three hundred–six hundred mg) is needed to gain therapeutic platelet inhibition extra hastily.
3. Irreversible Binding
While beneficial for sustained platelet inhibition, the irreversible binding poses a threat in sufferers who require pressing surgery or experience bleeding complications, as platelet function can only be restored via the technology of new platelets.
Clopidogrel in Comparison with Other P2Y12 Inhibitors
Two more moderen P2Y12 inhibitors—prasugrel and ticagrelor—have emerged as options to clopidogrel.
Prasugrel is stronger and has a faster onset; however, it incorporates a higher bleeding risk, specifically in patients with earlier stroke or low body weight.
Ticagrelor is a reversible P2Y12 inhibitor that doesn’t require metabolic activation. A few studies have shown advanced outcomes (e.g., the PLATO trial). However, it might also cause side effects, including dyspnea and bradyarrhythmias.
Despite these options, clopidogrel remains the drug of choice in many eventualities because of its decreased fee and safety in patients at excessive danger of bleeding.
Personalized Medicine and Genetic Testing
The variability in clopidogrel metabolism has led to a growing hobby in pharmacogenomic testing to guide antiplatelet therapy. The Clinical Pharmacogenetics Implementation Consortium (CPIC) recommends considering alternative marketers in CYP2C19 negative metabolizers.
Point-of-care genetic tests are becoming more accessible, permitting clinicians to tailor antiplatelet medication more accurately. However, routine genetic testing isn’t yet a preferred exercise due to cost, availability, and varying guidelines.
Drug Interactions and Contraindications
Clopidogrel’s efficacy can be stimulated by using co-administered pills. Notably:
Proton pump inhibitors (PPIs), such as Torsilax omeprazole, may also inhibit CYP2C19 and decrease clopidogrel activation. Alternatives like pantoprazole are often favored.
Drugs that inhibit or induce CYP enzymes can alter clopidogrel’s metabolism and effectiveness.
Clopidogrel is contraindicated in patients with active bleeding, hypersensitive reaction, or vast hepatic impairment.
Future Directions and Ongoing Research
Research is ongoing to optimize the use of clopidogrel in unique populations, including diabetics, those undergoing complex PCI, and patients with continual kidney sickness. Studies are also exploring combinations of low-dose anticoagulants and antiplatelet agents to stabilize efficacy and bleeding risk.
Efforts to increase novel P2Y12 inhibitors with better pharmacokinetic profiles and fewer side results continue. Meanwhile, real-international data and registry studies are helping refine danger stratification and treatment length techniques for clopidogrel remedy.
Deduction
Clopidogrel has solidified its function as a key participant in cardiovascular care through its effective platelet inhibition, established scientific blessings, and favorable safety profile. Despite the emergence of more recent agents and issues about genetic variability, clopidogrel remains a cornerstone in preventing and controlling thrombotic cardiovascular events.
Personalized methods, including pharmacogenomic testing and cautious patient choice, are enhancing its scientific utility. As cardiovascular medicine continues to adapt, clopidogrel stands as a testimony to the power of focused treatment in enhancing effects and saving lives.
